What is Bladder Cancer?
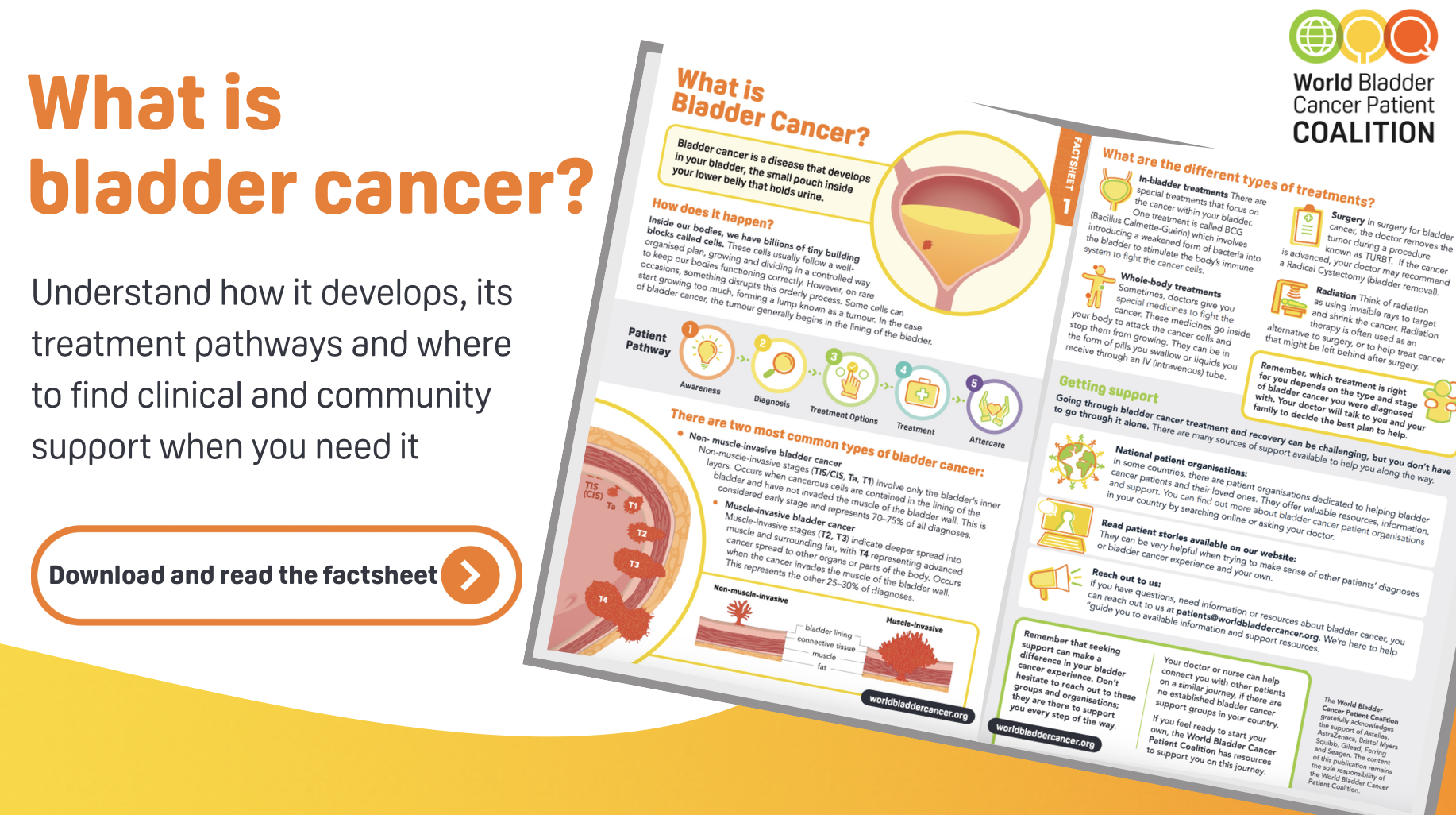
Bladder cancer is a disease that starts in the bladder, a small pouch in your lower belly that holds urine before it leaves your body.
Like all cancers, it happens when some of the body’s cells stop following their normal rules. Normally, our cells grow, divide, and die in an organised way to keep us healthy. But sometimes this process breaks down. Certain cells grow too quickly and do not die when they should. Over time, they can form a lump called a tumour.
In bladder cancer, tumours usually begin in the lining of the bladder, the inner surface that comes into contact with urine. Some tumours stay in this lining, while others can grow deeper into the muscle and wall of the bladder. The deeper the tumour grows, the harder it is to treat.
How does the bladder work?
To understand bladder cancer, it helps to know a little about how the bladder works.
- The kidneys act as natural filters. They clean your blood and remove waste, turning it into urine.
- The ureters are thin tubes that carry urine from the kidneys down into the bladder.
- The bladder itself is like a stretchy balloon made of muscle. It expands to store urine and contracts when it is time to empty it. Most people’s bladder can hold up to half a litre (about a pint) of urine.
- The urethra is the tube that carries urine out of the body.
Most of the inside of the urinary system is covered with a special lining of cells called transitional cells. This is the place where bladder cancer usually begins.
Types of bladder cancer
Doctors usually describe bladder cancer in two main groups. This depends on whether the cancer has spread into the bladder muscle or not.
Non-muscle-invasive bladder cancer (NMIBC)
This means the cancer cells are only in the inner lining of the bladder. They have not spread into the muscle of the bladder wall. This type is often found early and makes up about 70–75% of all cases.
- It includes stages Ta, T1, and TIS/CIS.
- Doctors usually call this “early stage” bladder cancer.
Muscle-invasive bladder cancer (MIBC)
This means the cancer has spread deeper into the muscle of the bladder wall, and sometimes into surrounding tissue. This type is more serious and makes up about 25–30% of cases.
- It includes stages T2, T3, and T4.
- At this stage, the cancer is more likely to spread to other organs.
Treatment options
The treatment that is right for you will depend on the type and stage of your bladder cancer, as well as your overall health. Your doctor will talk through the best plan for your situation.
Here are the main types of treatments:
In-bladder treatments
Some medicines are placed directly into the bladder through a thin tube (catheter).
- The most common is BCG (Bacillus Calmette-Guérin). This is a type of weakened bacteria that helps your immune system attack cancer cells.
Surgery
There are two main types of surgery for bladder cancer:
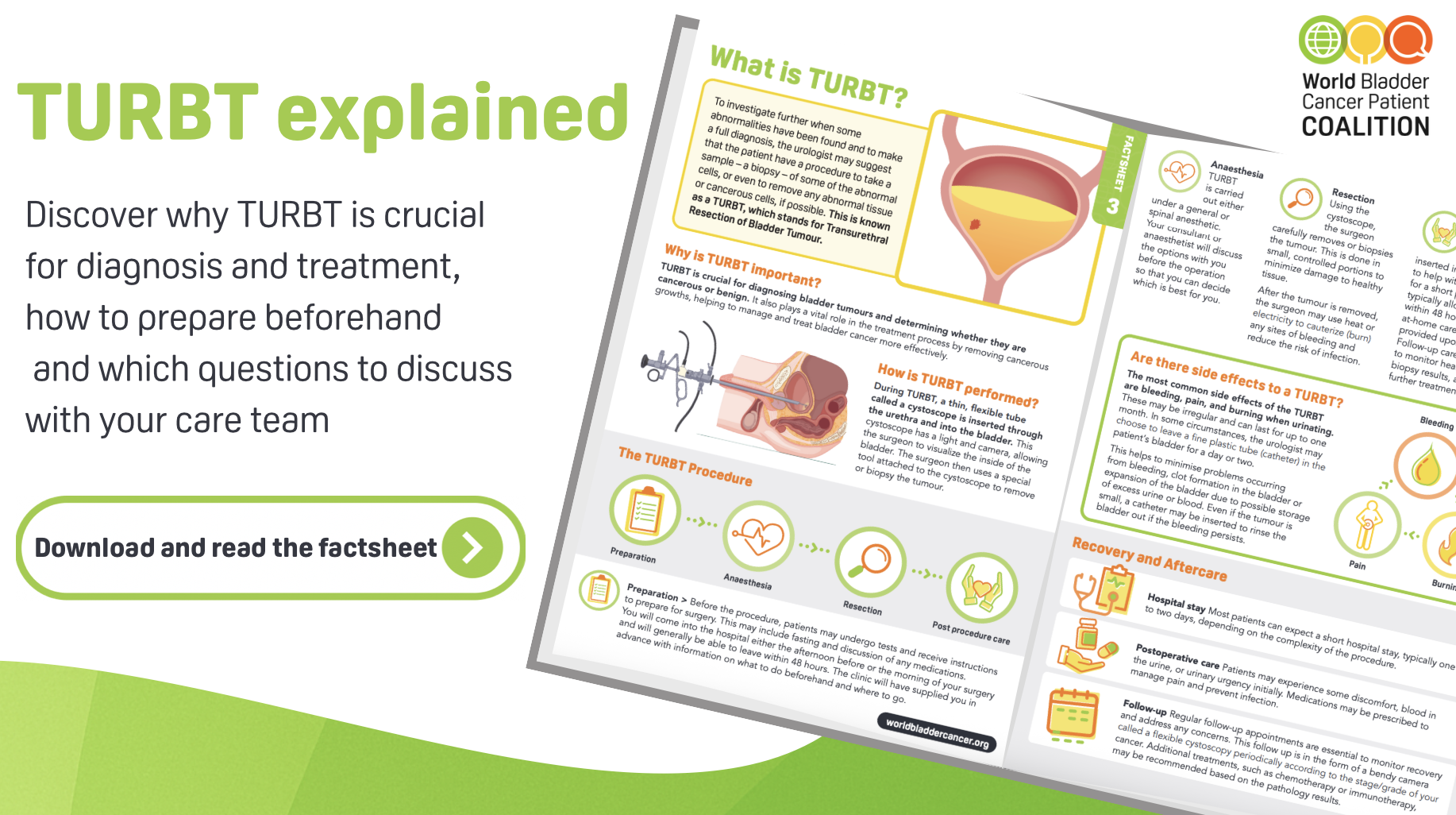
- TURBT (Transurethral Resection of Bladder Tumour): Doctors remove the tumour through the urethra without cutting open the body. This is often used for early-stage cancers.
- Radical cystectomy: In some advanced cases, the whole bladder may need to be removed. If this happens, doctors will create another way for urine to leave your body.
Whole-body treatments
Sometimes medicines are used to travel through your bloodstream and fight cancer cells all over the body.
- These include chemotherapy, immunotherapy, and targeted therapy. They may be given as tablets or through a drip (IV).
Radiation therapy
This uses high-energy beams to kill cancer cells or shrink tumours. It can be used instead of surgery, or together with other treatments to make them more effective.
Living with bladder cancer: finding support
A diagnosis of bladder cancer can feel overwhelming, but you don’t have to face it alone. Many sources of support are available:
- Patient organisations
In many countries, there are groups dedicated to helping bladder cancer patients and families. They can offer information, resources, and a community of people who understand what you are going through. - Patient stories
Reading about other people’s experiences can help you feel less alone and give you ideas for coping with your own journey. You can read real stories from patients on our patient stories page. - Reach out to us
If you have questions or need resources, you can contact us at patients@worldbladdercancer.org. We are here to connect you with information and support that may help you.
If there are no bladder cancer support groups in your country, your doctor or nurse may be able to connect you with other patients. And if you feel ready, the World Bladder Cancer Patient Coalition has resources to help you start a new support group in your community.
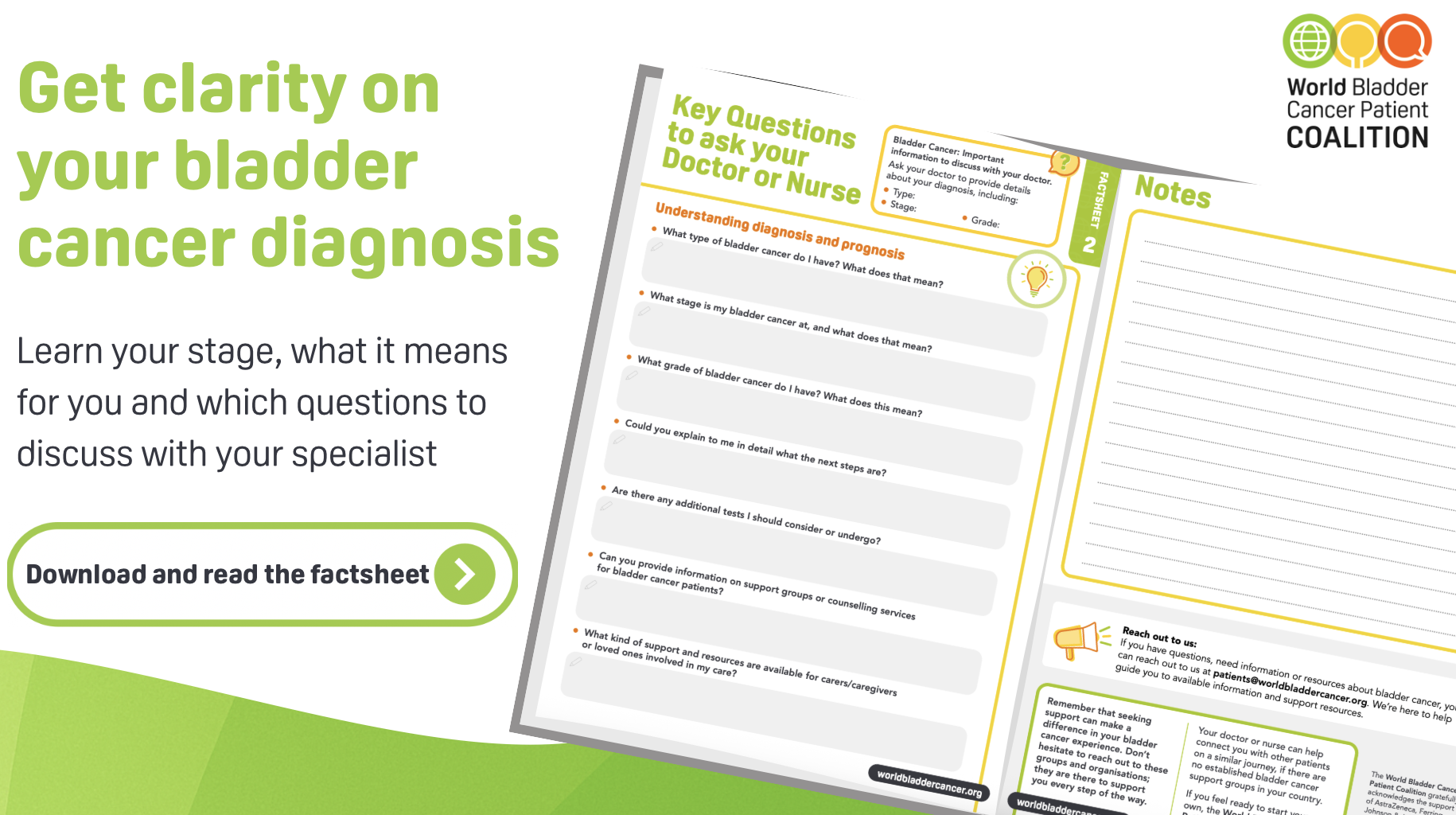
What are bladder cancer types, stages & grades?
Bladder cancer is usually divided into two groups:
- Non-muscle-invasive bladder cancer (NMIBC): Cancer is only in the inner lining of the bladder and has not grown into the muscle. This is the most common form.
- Muscle-invasive bladder cancer (MIBC): Cancer has spread into the muscle of the bladder wall or beyond. This type is more serious and needs stronger treatments.
This difference is very important, because it guides which treatment options are recommended.
Bladder tumours don’t all look or behave the same. Doctors often describe them as:
-
Papillary tumours
Grow out from the bladder lining on a stalk, like tiny fingers or warts. They usually grow into the bladder cavity, not into the deeper wall. -
Sessile tumours
Lie flat against the bladder lining. Because they spread wider and are harder to see, they are more likely to grow deeper into the bladder wall. -
Carcinoma in situ (CIS)
A flat tumour that looks like a red, inflamed patch on the bladder lining. CIS is a high-grade form of bladder cancer, meaning it is more likely to return or spread if not treated. Around 1 in 10 people with bladder cancer are diagnosed with CIS.
es. Most bladder cancers (90–95%) begin in the bladder itself. But the same type of lining cells (urothelial cells) are also found in the kidneys and ureters.
When cancer starts there, it is called upper tract urothelial carcinoma (UTUC).
-
In the renal pelvis (the part of the kidney where urine collects).
-
Or in the ureter (the tube that carries urine from the kidney to the bladder).
UTUC is much less common, but it is treated in similar ways to bladder cancer.
Stage tells us how far the cancer has grown. It shows whether the tumour is only in the bladder lining, has grown into the muscle, or has spread outside the bladder.
-
T0: No tumour is seen.
-
Ta: A papillary tumour that has not grown into the bladder wall.
-
TIS (CIS): Carcinoma in situ, a flat high-grade tumour limited to the lining.
-
T1: Tumour has grown into the connective tissue just under the lining.
-
T2: Tumour has grown into the bladder muscle.
-
T3: Tumour has gone through the bladder wall into the surrounding fat.
-
T4: Tumour has spread to nearby organs (like the prostate, uterus, vagina, or pelvic wall).
Grade describes how abnormal the cancer cells look and how quickly they might grow.
-
Low grade (G1): Cells look more like normal bladder cells. They tend to grow slowly and are less likely to spread.
-
High grade (G3): Cells look very different from normal. They grow faster and are more likely to come back or spread.
Doctors may simply say low grade or high grade rather than using numbers.
The type of tumour shows how the cancer behaves.
The stage shows how far it has grown or spread.
The grade shows how aggressive it is.
Together, these three factors help doctors choose the best treatment and predict how the cancer might develop in the future.